Cancer-specific treatment to weaken the cancer cells to improve immunotherapy-induced clearance.
Targeting E2N for Immuno-Cancer Therapy
Cancer-specific treatment to weaken the cancer cells to improve immunotherapy-induced clearance.
Cancer continues to account for ~20% of all deaths in men and women, placing a significant burden on the medical system. While immunotherapies have emerged as potential treatments, the treatment is not cell-specific, affecting cancerous and healthy tissues alike by modulating the body’s immune response. In an effort to improve the efficacy of immunotherapy, researchers at VCU have developed an additional treatment that is cancer-cell specific and designed to weaken cancer cells making them more vulnerable and visible to immunotherapy to better direct immune cells onto the cancer cells, improving their clearance from the patient’s body with efficacy proven in multiple cancer types.
The technology
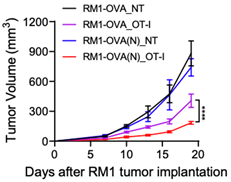
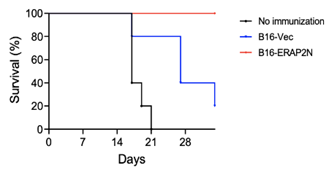
is an enzyme that trims antigenic peptides to be presented on the membrane. These membrane-bound antigens are presented to CD8+ T cells which specifically mark these cells for immune response. Providing E2N to cancer cells now exposes more membrane-bound antigens that normal/healthy cells do not present, increasing the likelihood that immunotherapy will preferentially remove cancer rather than healthy neighboring cells. Current immunotherapies attack both healthy and cancerous cells, which can cause complications. Thus, this vaccine-based therapy helps render prostate tumors susceptible to T-cell therapy by making the tumor cells more preferential for cytotoxic killing. (Figure 1) The E2N vaccine has also been shown to reduce prostate tumor volume by ~70% after twenty days of treatment compared to the untreated control group. (Figure 2) Additionally, the E2N vaccine “educates” the host immune cells to eliminate tumor growth thus increases survivability in melanoma cancer animal models. (Figure 3)
Figure 1. The cytotoxicity is significantly higher with RM1-OVA expressing (N) vs. RM1-OVA without (N).
Figure 2. The tumor volume decreased significantly with RM1-OVA(N) when treated with OVA-specific T cells (OT-1) compared to RM-1-OVA without (N) and untreated groups.
Figure 3. The E2N vaccine increased the survivability in a mouse animal model compared to vector and no vaccine control.